Abstract
Binge eating disorder (BED) is characterized by regular binge eating episodes during which individuals ingest comparably large amounts of food and experience loss of control over their eating behaviour. The worldwide prevalence of BED for the years 2018–2020 is estimated to be 0.6–1.8% in adult women and 0.3–0.7% in adult men. BED is commonly associated with obesity and with somatic and mental health comorbidities. People with BED experience considerable burden and impairments in quality of life, and, at the same time, BED often goes undetected and untreated. The aetiology of BED is complex, including genetic and environmental factors as well as neuroendocrinological and neurobiological contributions. Neurobiological findings highlight impairments in reward processing, inhibitory control and emotion regulation in people with BED, and these neurobiological domains are targets for emerging treatment approaches. Psychotherapy is the first-line treatment for BED. Recognition and research on BED has increased since its inclusion into DSM-5; however, continuing efforts are needed to understand underlying mechanisms of BED and to improve prevention and treatment outcomes for this disorder. These efforts should also include screening, identification and implementation of evidence-based interventions in routine clinical practice settings such as primary care and mental health outpatient clinics.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
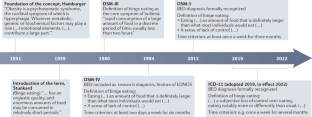
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 350–353 (American Psychiatric Association, 2013).
World Health Organization. ICD-11: International Classification of Diseases 11th Revision. ICD https://icd.who.int/ (2019).
Treasure, J. et al. Anorexia nervosa. Nat. Rev. Dis. Primers 1, 15074 (2015).
Zipfel, S., Giel, K. E., Bulik, C. M., Hay, P. & Schmidt, U. Anorexia nervosa: aetiology, assessment, and treatment. Lancet Psychiatry 2, 1099–1111 (2015).
Keski-Rahkonen, A. & Mustelin, L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr. Opin. Psychiatry 29, 340–345 (2016).
Hoek, H. W. Review of the worldwide epidemiology of eating disorders. Curr. Opin. Psychiatry 29, 336–339 (2016).
Udo, T. & Grilo, C. M. Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of U.S. adults. Biol. Psychiatry 84, 345–354 (2018).
Agh, T. et al. Epidemiology, health-related quality of life and economic burden of binge eating disorder: a systematic literature review. Eat. Weight. Disord. 20, 1–12 (2015). This systematic review highlights what is known about quality of life and burden of people affected by BED.
Dawes, A. J. et al. Mental health conditions among patients seeking and undergoing bariatric surgery: a meta-analysis. JAMA 315, 150–163 (2016).
NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387, 1377–1396 (2016).
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894 (WHO, 2000).
National Institute for Health and Care Excellence. Eating disorders: recognition and treatment (full guideline). NICE https://www.nice.org.uk/guidance/ng69/evidence/full-guideline-pdf-161214767896 (2017).
Herpertz, S. et al. S3-Leitlinie Diagnostik und Behandlung der Essstörungen. AWMF https://www.awmf.org/uploads/tx_szleitlinien/051-026l_S3_Essstoerung-Diagnostik-Therapie_2020-03.pdf (2018).
Gonzalez-Muniesa, P. et al. Obesity. Nat. Rev. Dis. Primers 3, 17034 (2017).
Santomauro, D. F. et al. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study 2019. Lancet Psychiatry 8, 320–328 (2021). This paper, based on studies from the Global Burden of Disease (GBD) dataset provides up-to-date evidence on epidemiology and burden caused by eating disorders including BED, providing so far unrepresented GBD data.
Stice, E., Marti, C. N. & Rohde, P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J. Abnorm. Psychol. 122, 445–457 (2013).
Kessler, R. C. et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol. Psychiatry 73, 904–914 (2013).
Keski-Rahkonen, A. Epidemiology of binge eating disorder: prevalence, course, comorbidity, and risk factors. Curr. Opin. Psychiatry 34, 525–531 (2021).
Mitchison, D. et al. DSM-5 full syndrome, other specified, and unspecified eating disorders in Australian adolescents: prevalence and clinical significance. Psychol. Med. 50, 981–990 (2020).
Olsen, E. M., Koch, S. V., Skovgaard, A. M. & Strandberg-Larsen, K. Self-reported symptoms of binge-eating disorder among adolescents in a community-based Danish cohort–a study of prevalence, correlates, and impact. Int. J. Eat. Disord. 54, 492–505 (2021).
Glazer, K. B. et al. The course of eating disorders involving bingeing and purging among adolescent girls: prevalence, stability, and transitions. J. Adolesc. Health 64, 165–171 (2019).
Meule, A. The psychology of overeating: food and the culture of consumerism. Food Cult. Soc. 19, 735–736 (2016).
Streatfeild, J. et al. Social and economic cost of eating disorders in the United States: evidence to inform policy action. Int. J. Eat. Disord. 54, 851–868 (2021).
Silén, Y. et al. Detection, treatment, and course of eating disorders in Finland: a population-based study of adolescent and young adult females and males. Eur. Eat. Disord. Rev. 29, 720–732 (2021).
Coffino, J. A., Udo, T. & Grilo, C. M. Rates of help-seeking in US adults with lifetime DSM-5 eating disorders: prevalence across diagnoses and differences by sex and ethnicity/race. Mayo Clin. Proc. 94, 1415–1426 (2019).
Abbott, S., Dindol, N., Tahrani, A. A. & Piya, M. K. Binge eating disorder and night eating syndrome in adults with type 2 diabetes: a systematic review. J. Eat. Disord. 6, 36 (2018).
Brownley, K. A. et al. Binge-eating disorder in adults: a systematic review and meta-analysis. Ann. Intern. Med. 165, 409–420 (2016).
Wassenaar, E., Friedman, J. & Mehler, P. S. Medical complications of binge eating disorder. Psychiatr. Clin. North. Am. 42, 275–286 (2019).
Harris, S. R., Carrillo, M. & Fujioka, K. Binge-eating disorder and type 2 diabetes: a review. Endocr. Pract. 27, 158–164 (2021).
Tate, A. E. et al. Association and familial coaggregation of type 1 diabetes and eating disorders: a register-based cohort study in Denmark and Sweden. Diabetes Care 44, 1143–1150 (2021).
Zhang, J. et al. Pilot study of the prevalence of binge eating disorder in non-alcoholic fatty liver disease patients. Ann. Gastroenterol. 30, 664–669 (2017).
Forlano, R. et al. Binge-eating disorder is associated with an unfavorable body mass composition in patients with non-alcoholic fatty liver disease. Int. J. Eat. Disord. 54, 2025–2030 (2021).
Cremonini, F. et al. Associations among binge eating behavior patterns and gastrointestinal symptoms: a population-based study. Int. J. Obes. 33, 342–353 (2009).
Thornton, L. M. et al. Binge-eating disorder in the Swedish national registers: somatic comorbidity. Int. J. Eat. Disord. 50, 58–65 (2017).
Kimmel, M. C., Ferguson, E. H., Zerwas, S., Bulik, C. M. & Meltzer-Brody, S. Obstetric and gynecologic problems associated with eating disorders. Int. J. Eat. Disord. 49, 260–275 (2016).
Udo, T. & Grilo, C. M. Psychiatric and medical correlates of DSM-5 eating disorders in a nationally representative sample of adults in the United States. Int. J. Eat. Disord. 52, 42–50 (2019). This paper provides a recent and comprehensive description of common co-occurring conditions with eating disorders based on a representative population sample.
Udo, T., Bitley, S. & Grilo, C. M. Suicide attempts in US adults with lifetime DSM-5 eating disorders. BMC Med. 17, 120–123 (2019).
Fernandez-Aranda, F. et al. Impulse control disorders in women with eating disorders. Psychiatry Res. 157, 147–157 (2008).
Jimenez-Murcia, S. et al. Pathological gambling in eating disorders: prevalence and clinical implications. Compr. Psychiatry 54, 1053–1060 (2013).
Nazar, B. P. et al. The risk of eating disorders comorbid with attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Int. J. Eat. Disord. 49, 1045–1057 (2016).
Schmidt, F., Körber, S., de Zwaan, M. & Müller, A. Impulse control disorders in obese patients. Eur. Eat. Disord. Rev. 20, e144–e147 (2012).
Lydecker, J. A. & Grilo, C. M. Psychiatric comorbidity as predictor and moderator of binge-eating disorder treatment outcomes: an analysis of aggregated randomized controlled trials. Psychol. Med. https://doi.org/10.1017/S0033291721001045 (2021).
West, C. E., Goldschmidt, A. B., Mason, S. M. & Neumark-Sztainer, D. Differences in risk factors for binge eating by socioeconomic status in a community-based sample of adolescents: findings from Project EAT. Int. J. Eat. Disord. 52, 659–668 (2019).
Braun, J. et al. Trauma exposure, DSM-5 posttraumatic stress, and binge eating symptoms: results from a nationally representative sample. J. Clin. Psychiatry 80, 19m12813 (2019).
Coffino, J. A., Udo, T. & Grilo, C. M. The significance of overvaluation of shape or weight in binge-eating disorder: results from a national sample of U.S. adults. Obesity 27, 1367–1371 (2019).
& Borg, S. L. et al. Relationships between childhood abuse and eating pathology among individuals with binge-eating disorder: examining the moderating roles of self-discrepancy and self-directed style. Eat. Disord. https://doi.org/10.1080/10640266.2020.1864588 (2021).
Hazzard, V. M., Bauer, K. W., Mukherjee, B., Miller, A. L. & Sonneville, K. R. Associations between childhood maltreatment latent classes and eating disorder symptoms in a nationally representative sample of young adults in the United States. Child. Abus. Negl. 98, 104171 (2019).
Hazzard, V. M., Loth, K. A., Hooper, L. & Becker, C. B. Food insecurity and eating disorders: a review of emerging evidence. Curr. Psychiatry Rep. 22, 74–70 (2020).
& Hazzard, V. M. et al. Past-year abuse and eating disorder symptoms among U.S. college students. J. Interpers. Violence https://doi.org/10.1177/08862605211005156 (2021).
Masheb, R. M. et al. DSM-5 eating disorder prevalence, gender differences, and mental health associations in United States military veterans. Int. J. Eat. Disord. 54, 1171–1180 (2021).
de Beaurepaire, R. Binge eating disorders in antipsychotic-treated patients with schizophrenia: prevalence, antipsychotic specificities, and changes over time. J. Clin. Psychopharmacol. 41, 114–120 (2021).
Goode, R. W. et al. Binge eating and binge-eating disorder in Black women: a systematic review. Int. J. Eat. Disord. 53, 491–507 (2020).
Marques, L. et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: implications for reducing ethnic disparities in health care access for eating disorders. Int. J. Eat. Disord. 44, 412–420 (2011).
Perez, M., Ohrt, T. K. & Hoek, H. W. Prevalence and treatment of eating disorders among Hispanics/Latino Americans in the United States. Curr. Opin. Psychiatry 29, 378–382 (2016).
Kamody, R. C., Grilo, C. M. & Udo, T. Disparities in DSM-5 defined eating disorders by sexual orientation among US adults. Int. J. Eat. Disord. 53, 278–287 (2020).
Nagata, J. M., Ganson, K. T. & Austin, S. B. Emerging trends in eating disorders among sexual and gender minorities. Curr. Opin. Psychiatry 33, 562–567 (2020).
Beccia, A. L., Baek, J., Austin, S. B., Jesdale, W. M. & Lapane, K. L. Eating-related pathology at the intersection of gender, gender expression, sexual orientation, and weight status: an intersectional Multilevel Analysis of Individual Heterogeneity and Discriminatory Accuracy (MAIHDA) of the Growing Up Today Study cohorts. Soc. Sci. Med. 281, 114092 (2021).
Cheah, S. L., Jackson, E., Touyz, S. & Hay, P. Prevalence of eating disorder is lower in migrants than in the Australian-born population. Eat. Behav. 37, 101370 (2020).
Burt, A., Mitchison, D., Doyle, K. & Hay, P. Eating disorders amongst Aboriginal and Torres Strait Islander Australians: a scoping review. J. Eat. Disord. 8, 73 (2020).
Puhl, R. & Suh, Y. Health consequences of weight stigma: implications for obesity prevention and treatment. Curr. Obes. Rep. 4, 182–190 (2015).
Donnelly, B. et al. Neuroimaging in bulimia nervosa and binge eating disorder: a systematic review. J. Eat. Disord. 6, 3 (2018).
Strubbe, J. H. & Woods, S. C. The timing of meals. Psychol. Rev. 111, 128–141 (2004).
Berthoud, H. R. & Morrison, C. The brain, appetite, and obesity. Annu. Rev. Psychol. 59, 55–92 (2008).
Rosenbaum, M. & Leibel, R. L. 20 years of leptin: role of leptin in energy homeostasis in humans. J. Endocrinol. 223, T83–T96 (2014).
Muller, T. D. et al. Glucagon-like peptide 1 (GLP-1). Mol. Metab. 30, 72–130 (2019).
Yu, Y., Fernandez, I. D., Meng, Y., Zhao, W. & Groth, S. W. Gut hormones, adipokines, and pro- and anti-inflammatory cytokines/markers in loss of control eating: a scoping review. Appetite 166, 105442 (2021).
Hernandez, D., Mehta, N. & Geliebter, A. Meal-related acyl and des-acyl ghrelin and other appetite-related hormones in people with obesity and binge eating. Obesity 27, 629–635 (2019).
Munsch, S., Biedert, E., Meyer, A. H., Herpertz, S. & Beglinger, C. CCK, ghrelin, and PYY responses in individuals with binge eating disorder before and after a cognitive behavioral treatment (CBT). Physiol. Behav. 97, 14–20 (2009).
Voon, V. Cognitive biases in binge eating disorder: the hijacking of decision making. CNS Spectr. 20, 566–573 (2015).
Avena, N. M., Bocarsly, M. E., Hoebel, B. G. & Gold, M. S. Overlaps in the nosology of substance abuse and overeating: the translational implications of “food addiction”. Curr. Drug Abus. Rev. 4, 133–139 (2011).
& Steward, T. et al. What difference does it make? Risk-taking behavior in obesity after a loss is associated with decreased ventromedial prefrontal cortex activity. J. Clin. Med. 8, 1551 (2019).
Hege, M. A. et al. Attentional impulsivity in binge eating disorder modulates response inhibition performance and frontal brain networks. Int. J. Obes. 39, 353–360 (2015).
Wolz, I. et al. Subjective craving and event-related brain response to olfactory and visual chocolate cues in binge-eating and healthy individuals. Sci. Rep. 7, 41736 (2017).
Balodis, I. M. et al. Divergent neural substrates of inhibitory control in binge eating disorder relative to other manifestations of obesity. Obesity 21, 367–377 (2013).
Frank, G. K. W., Shott, M. E., Stoddard, J., Swindle, S. & Pryor, T. L. Association of brain reward response with body mass index and ventral striatal-hypothalamic circuitry among young women with eating disorders. JAMA Psychiatry 78, 1123–1133 (2021).
Leehr, E. J. et al. Emotion regulation model in binge eating disorder and obesity–a systematic review. Neurosci. Biobehav. Rev. 49, 125–134 (2015).
Ansell, E. B., Grilo, C. M. & White, M. A. Examining the interpersonal model of binge eating and loss of control over eating in women. Int. J. Eat. Disord. 45, 43–50 (2012).
Iceta, S. et al. Cognitive function in binge eating disorder and food addiction: a systematic review and three-level meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 111, 110400 (2021).
Giel, K. E., Teufel, M., Junne, F., Zipfel, S. & Schag, K. Food-related impulsivity in obesity and binge eating disorder–a systematic update of the evidence. Nutrients 9, 1170 (2017).
Kessler, R. M., Hutson, P. H., Herman, B. K. & Potenza, M. N. The neurobiological basis of binge-eating disorder. Neurosci. Biobehav. Rev. 63, 223–238 (2016). This review provides a comprehensive synthesis of the neurobiological findings in BED and develops hyopotheses for neurobiological pathomechanisms in the development and maintenance of BED.
Schag, K., Schonleber, J., Teufel, M., Zipfel, S. & Giel, K. E. Food-related impulsivity in obesity and binge eating disorder–a systematic review. Obes. Rev. 14, 477–495 (2013).
Mallorqui-Bague, N. et al. Impulsivity and cognitive distortions in different clinical phenotypes of gambling disorder: profiles and longitudinal prediction of treatment outcomes. Eur. Psychiatry 61, 9–16 (2019).
& Lozano-Madrid, et al.Impulsivity, emotional dysregulation and executive function deficits could be associated with alcohol and drug abuse in eating disorders. J. Clin. Med. 9, 1936 (2020).
Grant, J. E. & Chamberlain, S. R. Neurocognitive findings in young adults with binge eating disorder. Int. J. Psychiatry Clin. Pract. 24, 71–76 (2020).
Oliva, R., Morys, F., Horstmann, A., Castiello, U. & Begliomini, C. Characterizing impulsivity and resting-state functional connectivity in normal-weight binge eaters. Int. J. Eat. Disord. 53, 478–488 (2020).
Lucas, I. et al. Neuropsychological learning deficits as predictors of treatment outcome in patients with eating disorders. Nutrients 13, 2145 (2021).
Schag, K. et al. Food-related impulsivity assessed by longitudinal laboratory tasks is reduced in patients with binge eating disorder in a randomized controlled trial. Sci. Rep. 11, 8225 (2021).
Dingemans, A. E., van Son, G. E., Vanhaelen, C. B. & van Furth, E. F. Depressive symptoms rather than executive functioning predict group cognitive behavioural therapy outcome in binge eating disorder. Eur. Eat. Disord. Rev. 28, 620–632 (2020).
Mestre-Bach, G., Fernandez-Aranda, F., Jimenez-Murcia, S. & Potenza, M. N. Decision-making in gambling disorder, problematic pornography use, and binge-eating disorder: similarities and differences. Curr. Behav. Neurosci. Rep. 7, 97–108 (2020).
Amlung, M. et al. Delay discounting as a transdiagnostic process in psychiatric disorders: a meta-analysis. JAMA Psychiatry 76, 1176–1186 (2019).
Appelhans, B. M. et al. Inhibiting food reward: delay discounting, food reward sensitivity, and palatable food intake in overweight and obese women. Obesity 19, 2175–2182 (2011).
Tang, J., Chrzanowski-Smith, O. J., Hutchinson, G., Kee, F. & Hunter, R. F. Relationship between monetary delay discounting and obesity: a systematic review and meta-regression. Int. J. Obes. 43, 1135–1146 (2019).
Steward, T. et al. Delay discounting of reward and impulsivity in eating disorders: from anorexia nervosa to binge eating disorder. Eur. Eat. Disord. Rev. 25, 601–606 (2017).
Steward, T. et al. Delay discounting and impulsivity traits in young and older gambling disorder patients. Addict. Behav. 71, 96–103 (2017).
Miranda-Olivos, R. et al. The neural correlates of delay discounting in obesity and binge eating disorder. J. Behav. Addict. 10, 498–507 (2021).
Fowler, S. & Bulik, C. Family environment and psychiatric history in women with binge eating disorder and obese controls. Behav. Change 14, 106–112 (1997).
Hudson, J. et al. Familial aggregation of binge-eating disorder. Arch. Gen. Psychiatry 63, 313–319 (2006).
Javaras, K. N. et al. Familiality and heritability of binge eating disorder: results of a case-control family study and a twin study. Int. J. Eat. Disord. 41, 174–179 (2008).
Mitchell, K. S. et al. Binge eating disorder: a symptom-level investigation of genetic and environmental influences on liability. Psychol. Med. 40, 1899–1906 (2010).
Reichborn-Kjennerud, T., Bulik, C., Tambs, K. & Harris, J. Genetic and environmental influences on binge eating in the absence of compensatory behaviours: a population-based twin study. Int. J. Eat. Disord. 36, 307–314 (2004).
Manfredi, L., Accoto, A., Couyoumdjian, A. & Conversi, D. A systematic review of genetic polymorphisms associated with binge eating disorder. Nutrients 13, 848 (2021).
Micioni Di Bonaventura, E. et al. The melanocortin system behind the dysfunctional eating behaviors. Nutrients 12, 3502 (2020).
Qasim, A. et al. Gain-of-function variants in the melanocortin 4 receptor gene confer susceptibility to binge eating disorder in subjects with obesity: a systematic review and meta-analysis. Obes. Rev. 20, 13–21 (2019).
Hübel, C. et al. One size does not fit all. Genomics differentiates among anorexia nervosa, bulimia nervosa, and binge-eating disorder. Int. J. Eat. Disord. 54, 785–793 (2021). This study uses data from the UK Biobank to present the first molecular genetic evidence that the underlying biology differs between binge-type eating disorders, including bulimia nervosa and binge-eating disorder and anorexia nervosa, and these differences can be captured at the genomic level.
Dinan, T. G. & Cryan, J. F. The impact of gut microbiota on brain and behaviour: implications for psychiatry. Curr. Opin. Clin. Nutr. Metab. Care 18, 552–558 (2015).
Basolo, A. et al. Effects of underfeeding and oral vancomycin on gut microbiome and nutrient absorption in humans. Nat. Med. 26, 589–598 (2020).
David, L. A. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505, 559–563 (2014).
Wu, G. D. et al. Linking long-term dietary patterns with gut microbial enterotypes. Science 334, 105–108 (2011).
Ridaura, V. K. et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341, 1241214 (2013).
Chen, L. L. et al. Gut microbiota in psychiatric disorders: a systematic review. Psychosom. Med. 83, 679–692 (2021).
Reed, K. K., Abbaspour, A., Bulik, C. M. & Carroll, I. M. The intestinal microbiota and anorexia nervosa: cause or consequence of nutrient deprivation? Curr. Opin. Endocr. Metab. Res. 19, 46–51 (2021).
Herman, A. & Bajaka, A. The role of the intestinal microbiota in eating disorders–bulimia nervosa and binge eating disorder. Psychiatry Res. 300, 113923 (2021).
Alcock, J., Maley, C. C. & Aktipis, C. A. Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. Bioessays 36, 940–949 (2014).
van de Wouw, M., Schellekens, H., Dinan, T. G. & Cryan, J. F. Microbiota-gut-brain axis: modulator of host metabolism and appetite. J. Nutr. 147, 727–745 (2017).
Glenny, E. M., Bulik-Sullivan, E. C., Tang, Q., Bulik, C. M. & Carroll, I. M. Eating disorders and the intestinal microbiota: mechanisms of energy homeostasis and behavioral influence. Curr. Psychiatry Rep. 19, 51 (2017).
Madison, A. & Kiecolt-Glaser, J. K. Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr. Opin. Behav. Sci. 28, 105–110 (2019).
Rantala, M. J., Luoto, S., Krama, T. & Krams, I. Eating disorders: an evolutionary psychoneuroimmunological approach. Front. Psychol. 10, 2200 (2019).
Leyrolle, Q. et al. Specific gut microbial, biological, and psychiatric profiling related to binge eating disorders: a cross-sectional study in obese patients. Clin. Nutr. 40, 2035–2044 (2021).
Reas, D. L. Public and healthcare professionals’ knowledge and attitudes toward binge eating disorder: a narrative review. Nutrients 9, 1267 (2017).
Kazdin, A. E., Fitzsimmons-Craft, E. E. & Wilfley, D. E. Addressing critical gaps in the treatment of eating disorders. Int. J. Eat. Disord. 50, 170–189 (2017).
Kornstein, S. G. Epidemiology and recognition of binge-eating disorder in psychiatry and primary care. J. Clin. Psychiatry 78 (Suppl. 1), 3–8 (2017).
Wolfe, B. E., Baker, C. W., Smith, A. T. & Kelly-Weeder, S. Validity and utility of the current definition of binge eating. Int. J. Eat. Disord. 42, 674–686 (2009).
Lindvall Dahlgren, C. & Wisting, L. Transitioning from DSM-IV to DSM-5: a systematic review of eating disorder prevalence assessment. Int. J. Eat. Disord. 49, 975–997 (2016).
Dakanalis, A., Colmegna, F., Riva, G. & Clerici, M. Validity and utility of the DSM-5 severity specifier for binge-eating disorder. Int. J. Eat. Disord. 50, 917–923 (2017).
Grilo, C. M., Ivezaj, V. & White, M. A. Evaluation of the DSM-5 severity indicator for binge eating disorder in a clinical sample. Behav. Res. Ther. 71, 110–114 (2015).
Ali, K. et al. Perceived barriers and facilitators towards help-seeking for eating disorders: a systematic review. Int. J. Eat. Disord. 50, 9–21 (2017).
Bohon, C. Binge eating disorder in children and adolescents. Child. Adolesc. Psychiatr. Clin. N. Am. 28, 549–555 (2019).
Citrome, L. Binge eating disorder revisited: what’s new, what’s different, what’s next. CNS Spectr. 24, 4–13 (2019).
Morgan, J. F., Reid, F. & Lacey, J. H. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ 319, 1467–1468 (1999).
Parker, K. & Brennan, L. Measurement of disordered eating in bariatric surgery candidates: a systematic review of the literature. Obes. Res. Clin. Pract. 9, 12–25 (2015).
Klein, D. A., Sylvester, J. E. & Schvey, N. A. Eating disorders in primary care: diagnosis and management. Am. Fam. Physician 103, 22–32 (2021).
O’Loghlen, E., Grant, S. & Galligan, R. Shame and binge eating pathology: a systematic review. Clin. Psychol. Psychother. https://doi.org/10.1002/cpp.2615 (2021).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
Heriseanu, A. I., Hay, P., Corbit, L. & Touyz, S. Grazing in adults with obesity and eating disorders: a systematic review of associated clinical features and meta-analysis of prevalence. Clin. Psychol. Rev. 58, 16–32 (2017).
Pope, H. G. Jr. et al. Binge eating disorder: a stable syndrome. Am. J. Psychiatry 163, 2181–2183 (2006).
Wadden, T. A., Brownell, K. D. & Foster, G. D. Obesity: responding to the global epidemic. J. Consult. Clin. Psychol. 70, 510–525 (2002).
Kass, A. E. et al. Universal prevention efforts should address eating disorder pathology across the weight spectrum: implications for screening and intervention on college campuses. Eat. Behav. 25, 74–80 (2017).
Ewart-Pierce, E., Mejia Ruiz, M. J. & Gittelsohn, J. “Whole-of-community” obesity prevention: a review of challenges and opportunities in multilevel, multicomponent interventions. Curr. Obes. Rep. 5, 361–374 (2016).
Swinburn, B., Egger, G. & Raza, F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev. Med. 29, 563–570 (1999).
Booth, S. L. et al. Environmental and societal factors affect food choice and physical activity: rationale, influences, and leverage points. Nutr. Rev. 59, S21–S39; discussion S57–S65 (2001).
Micha, R. et al. Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLoS ONE 13, e0194555 (2018).
Pike, K. M. et al. Antecedent life events of binge-eating disorder. Psychiatry Res. 142, 19–29 (2006).
Stice, E., Desjardins, C. D., Rohde, P. & Shaw, H. Sequencing of symptom emergence in anorexia nervosa, bulimia nervosa, binge eating disorder, and purging disorder and relations of prodromal symptoms to future onset of these disorders. J. Abnorm. Psychol. 130, 377–387 (2021).
Harrer, M. et al. Internet interventions for mental health in university students: a systematic review and meta-analysis. Int. J. Methods Psychiatr. Res. 28, e1759 (2019).
Le, L. K., Barendregt, J. J., Hay, P. & Mihalopoulos, C. Prevention of eating disorders: a systematic review and meta-analysis. Clin. Psychol. Rev. 53, 46–58 (2017).
Stice, E., Onipede, Z. A. & Marti, C. N. A meta-analytic review of trials that tested whether eating disorder prevention programs prevent eating disorder onset. Clin. Psychol. Rev. 87, 102046 (2021).
Hay, P. et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust. N. Z. J. Psychiatry 48, 977–1008 (2014).
Hilbert, A., Hoek, H. W. & Schmidt, R. Evidence-based clinical guidelines for eating disorders: international comparison. Curr. Opin. Psychiatry 30, 423–437 (2017).
Peat, C. M. et al. Comparative effectiveness of treatments for binge-eating disorder: systematic review and network meta-analysis. Eur. Eat. Disord. Rev. 25, 317–328 (2017).
Hay, P. J. et al. Inpatient versus outpatient care, partial hospitalisation and waiting list for people with eating disorders. Cochrane Database Syst. Rev. 1, CD010827 (2019).
Fairburn, C. G. Cognitive Behavior Therapy and Eating Disorders (Guilford Press, 2008).
Wilfley, D. E., Mackenzie, K. R., Welch, R. R., Ayres, V. E. & Weissman, M. M. Interpersonal Psychotherapy for Group (Basic Books, 2008).
Safer, D. L., Telch, C. F. & Chen, E. Y. Dialectical Behavior Therapy for Binge Eating and Bulimia (Guilford Press, 2009).
Wilson, G. T. & Zandberg, L. J. Cognitive-behavioral guided self-help for eating disorders: effectiveness and scalability. Clin. Psychol. Rev. 32, 343–357 (2012).
Kenny, T. E., Carter, J. C. & Safer, D. L. Dialectical behavior therapy guided self-help for binge-eating disorder. Eat. Disord. 28, 202–211 (2020).
Hilbert, A. et al. Meta-analysis of the efficacy of psychological and medical treatments for binge-eating disorder. J. Consult. Clin. Psychol. 87, 91–105 (2019).
Wilson, G. T., Wilfley, D. E., Agras, W. S. & Bryson, S. W. Psychological treatments of binge eating disorder. Arch. Gen. Psychiatry 67, 94–101 (2010).
Hilbert, A. et al. Long-term efficacy of psychological treatments for binge eating disorder. Br. J. Psychiatry 200, 232–237 (2012).
Rozakou-Soumalia, N., Darvariu, S. & Sjogren, J. M. Dialectical behaviour therapy improves emotion dysregulation mainly in binge eating disorder and bulimia nervosa: a systematic review and meta-analysis. J. Pers. Med. 11, 931 (2021).
Lammers, M. W., Vroling, M. S., Crosby, R. D. & van Strien, T. Dialectical behavior therapy adapted for binge eating compared to cognitive behavior therapy in obese adults with binge eating disorder: a controlled study. J. Eat. Disord. 8, 27 (2020).
Vall, E. & Wade, T. D. Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. Int. J. Eat. Disord. 48, 946–971 (2015). This review and meta-analysis provides comprehensive information on predictors of outcome in the treatment of eating disorders.
Grilo, C. M., Thompson-Brenner, H., Shingleton, R. M., Thompson, D. R. & Franko, D. L. Clinical moderators and predictors of cognitive-behavioral therapy by guided-self-help versus therapist-led for binge-eating disorder: analysis of aggregated clinical trials. Int. J. Eat. Disord. 54, 1875–1880 (2021).
Hazzard, V. M. et al. Treatment outcomes of psychotherapy for binge-eating disorder in a randomized controlled trial: examining the roles of childhood abuse and post-traumatic stress disorder. Eur. Eat. Disord. Rev. 29, 611–621 (2021).
Hilbert, A. et al. Meta-analysis on the long-term effectiveness of psychological and medical treatments for binge-eating disorder. Int. J. Eat. Disord. 53, 1353–1376 (2020). This meta-analysis synthesizes current evidence on the efficacy of psychotherapy and pharmacotherapy for the treatment of BED.
Ghaderi, A. et al. Psychological, pharmacological, and combined treatments for binge eating disorder: a systematic review and meta-analysis. PeerJ 6, e5113 (2018).
Reas, D. L. & Grilo, C. M. Psychotherapy and medications for eating disorders: better together? Clin. Ther. 43, 17–39 (2021).
Heo, Y. A. & Duggan, S. T. Lisdexamfetamine: a review in binge eating disorder. CNS Drugs 31, 1015–1022 (2017).
Gasior, M. et al. A phase 3, multicenter, open-label, 12-month extension safety and tolerability trial of lisdexamfetamine dimesylate in adults with binge eating disorder. J. Clin. Psychopharmacol. 37, 315–322 (2017).
Hudson, J. I., McElroy, S. L., Ferreira-Cornwell, M. C., Radewonuk, J. & Gasior, M. Efficacy of lisdexamfetamine in adults with moderate to severe binge-eating disorder: a randomized clinical trial. JAMA Psychiatry 74, 903–910 (2017).
Grilo, C. M. et al. Efficacy and safety of dasotraline in adults with binge-eating disorder: a randomized, placebo-controlled, fixed-dose clinical trial. CNS Spectr. 26, 481–490 (2021).
McElroy, S. L. et al. Efficacy and safety of dasotraline in adults with binge-eating disorder: a randomized, placebo-controlled, flexible-dose clinical trial. J. Clin. Psychiatry 81, 19m13068 (2020).
Palavras, M. A., Hay, P., Filho, C. A. & Claudino, A. The efficacy of psychological therapies in reducing weight and binge eating in people with bulimia nervosa and binge eating disorder who are overweight or obese–a critical synthesis and meta-analyses. Nutrients 9, 299 (2017).
Munsch, S., Meyer, A. H. & Biedert, E. Efficacy and predictors of long-term treatment success for cognitive-behavioral treatment and behavioral weight-loss-treatment in overweight individuals with binge eating disorder. Behav. Res. Ther. 50, 775–785 (2012).
Ulian, M. D. et al. Effects of health at every size(R) interventions on health-related outcomes of people with overweight and obesity: a systematic review. Obes. Rev. 19, 1659–1666 (2018).
Grilo, C. M. et al. Randomized controlled trial testing the effectiveness of adaptive “SMART” stepped-care treatment for adults with binge-eating disorder comorbid with obesity. Am. Psychol. 75, 204–218 (2020).
Palavras, M. A. et al. Integrated weight loss and cognitive behavioural therapy (CBT) for the treatment of recurrent binge eating and high body mass index: a randomized controlled trial. Eat. Weight. Disord. 26, 249–262 (2021).
David, L. A., Sijercic, I. & Cassin, S. E. Preoperative and post-operative psychosocial interventions for bariatric surgery patients: a systematic review. Obes. Rev. 21, e12926 (2020).
Kops, N. L. et al. Preoperative binge eating and weight loss after bariatric surgery: a systematic review and meta-analysis. Obes. Surg. 31, 1239–1248 (2021).
Spirou, D., Raman, J. & Smith, E. Psychological outcomes following surgical and endoscopic bariatric procedures: a systematic review. Obes. Rev. 21, e12998 (2020).
Taba, J. V. et al. The development of feeding and eating disorders after bariatric surgery: a systematic review and meta-analysis. Nutrients 13, 2396 (2021).
Masheb, R. M., Dorflinger, L. M., Rolls, B. J., Mitchell, D. C. & Grilo, C. M. Binge abstinence is associated with reduced energy intake after treatment in patients with binge eating disorder and obesity. Obesity 24, 2491–2496 (2016).
Pacanowski, C. R. et al. Weight change over the course of binge eating disorder treatment: relationship to binge episodes and psychological factors. Obesity 26, 838–844 (2018).
Preuss, H., Pinnow, M., Schnicker, K. & Legenbauer, T. Improving inhibitory control abilities (ImpulsE)–a promising approach to treat impulsive eating? Eur. Eat. Disord. Rev. 25, 533–543 (2017).
Schag, K. et al. IMPULS: impulsivity-focused group intervention to reduce binge eating episodes in patients with binge eating disorder–a randomised controlled trial. Psychother. Psychosom. 88, 141–153 (2019).
Eichen, D. M., Matheson, B. E., Appleton-Knapp, S. L. & Boutelle, K. N. Neurocognitive treatments for eating disorders and obesity. Curr. Psychiatry Rep. 19, 62 (2017).
Ince, B. et al. Can we change binge eating behaviour by interventions addressing food-related impulsivity? A systematic review. J. Eat. Disord. 9, 38 (2021).
Raman, J., Hay, P., Tchanturia, K. & Smith, E. A randomised controlled trial of manualized cognitive remediation therapy in adult obesity. Appetite 123, 269–279 (2018).
Brockmeyer, T. et al. Approach bias modification training in bulimia nervosa and binge-eating disorder: a pilot randomized controlled trial. Int. J. Eat. Disord. 52, 520–529 (2019).
Chami, R. et al. Targeting binge eating in bulimia nervosa and binge eating disorder using inhibitory control training and implementation intentions: a feasibility trial. Psychol. Med. https://doi.org/10.1017/S0033291720002494 (2020).
Giel, K. E., Speer, E., Schag, K., Leehr, E. J. & Zipfel, S. Effects of a food-specific inhibition training in individuals with binge eating disorder–findings from a randomized controlled proof-of-concept study. Eat. Weight. Disord. 22, 345–351 (2017).
Lewer, M. et al. Effects of a cognitive-behavioral exposure-based body image therapy for overweight females with binge eating disorder: a pilot study. J. Eat. Disord. 5, 43 (2017).
Schyns, G., van den Akker, K., Roefs, A., Houben, K. & Jansen, A. Exposure therapy vs lifestyle intervention to reduce food cue reactivity and binge eating in obesity: a pilot study. J. Behav. Ther. Exp. Psychiatry 67, 101453 (2020).
Low, T. L., Ho, R., Ho, C. & Tam, W. The efficacy of virtual reality in the treatment of binge-purging eating disorders: a meta-analysis. Eur. Eat. Disord. Rev. 29, 52–59 (2021).
Manzoni, G. M. et al. Virtual reality-enhanced cognitive-behavioral therapy for morbid obesity: a randomized controlled study with 1 year follow-up. Cyberpsychol Behav. Soc. Netw. 19, 134–140 (2016).
Peterson, C. B. et al. Comparing integrative cognitive-affective therapy and guided self-help cognitive-behavioral therapy to treat binge-eating disorder using standard and naturalistic momentary outcome measures: a randomized controlled trial. Int. J. Eat. Disord. 53, 1418–1427 (2020).
Runfola, C. D. et al. A pilot open trial of UNITE-BED: a couple-based intervention for binge-eating disorder. Int. J. Eat. Disord. 51, 1107–1112 (2018).
Chao, A. M. et al. Effects of liraglutide and behavioral weight loss on food cravings, eating behaviors, and eating disorder psychopathology. Obesity 27, 2005–2010 (2019).
Da Porto, A. et al. Dulaglutide reduces binge episodes in type 2 diabetic patients with binge eating disorder: a pilot study. Diabetes Metab. Syndr. 14, 289–292 (2020).
Dalton, B., Bartholdy, S., Campbell, I. C. & Schmidt, U. Neurostimulation in clinical and sub-clinical eating disorders: a systematic update of the literature. Curr. Neuropharmacol. 16, 1174–1192 (2018).
Dalton, B., Campbell, I. C. & Schmidt, U. Neuromodulation and neurofeedback treatments in eating disorders and obesity. Curr. Opin. Psychiatry 30, 458–473 (2017).
Zeng, B. Y. et al. Efficacy and acceptability of noninvasive brain stimulation interventions for weight reduction in obesity: a pilot network meta-analysis. Int. J. Obes. 45, 1705–1716 (2021).
Max, S. M., Plewnia, C., Zipfel, S., Giel, K. E. & Schag, K. Combined antisaccade task and transcranial direct current stimulation to increase response inhibition in binge eating disorder. Eur. Arch. Psychiatry Clin. Neurosci. 271, 17–28 (2021).
Gordon, G., Brockmeyer, T., Schmidt, U. & Campbell, I. C. Combining cognitive bias modification training (CBM) and transcranial direct current stimulation (tDCS) to treat binge eating disorder: study protocol of a randomised controlled feasibility trial. BMJ Open 9, e030023 (2019).
WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 28, 551–558 (1998).
Topp, C. W., Ostergaard, S. D., Sondergaard, S. & Bech, P. The WHO-5 well-being index: a systematic review of the literature. Psychother. Psychosom. 84, 167–176 (2015).
Ware, J. Jr, Kosinski, M. & Keller, S. D. A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med. Care 34, 220–233 (1996).
Bohn, K. & Fairburn, C. in Cognitive Behavior Therapy and Eating Disorders: The Clinical Impairment Assessment Questionnaire (CIA). Appendix III (ed. Fairburn, C. G.) (Guilford Press, 2008).
Sepulveda, A. R., Whitney, J., Hankins, M. & Treasure, J. Development and validation of an Eating Disorders Symptom Impact Scale (EDSIS) for carers of people with eating disorders. Health Qual. Life Outcomes 6, 28 (2008).
Li, N., Mitchison, D., Touyz, S. & Hay, P. Cross-sectional comparison of health-related quality of life and other features in people with and without objective and subjective binge eating using a general population sample. BMJ Open 9, e024227 (2019).
Le, L. K. et al. Burden and health state utility values of eating disorders: results from a population-based survey. Psychol. Med. 51, 130–137 (2021). This paper provides important data on the burden associated with BED, which is based on a representative population sample.
Tannous, W. K. et al. The economic cost of bulimia nervosa and binge eating disorder: a population-based study. Psychol. Med. https://doi.org/10.1017/S0033291721000775 (2021).
Watson, H. J. et al. A register-based case-control study of health care utilization and costs in binge-eating disorder. J. Psychosom. Res. 108, 47–53 (2018).
Hart, L. M., Granillo, M. T., Jorm, A. F. & Paxton, S. J. Unmet need for treatment in the eating disorders: a systematic review of eating disorder specific treatment seeking among community cases. Clin. Psychol. Rev. 31, 727–735 (2011).
Hay, P. et al. General practitioner and mental healthcare use in a community sample of people with diagnostic threshold symptoms of bulimia nervosa, binge-eating disorder, and other eating disorders. Int. J. Eat. Disord. 53, 61–68 (2020).
Gearhardt, A. N. & Schulte, E. M. Is food addictive? A review of the science. Annu. Rev. Nutr. 41, 387–410 (2021).
Hebebrand, J. et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci. Biobehav. Rev. 47, 295–306 (2014).
van Hoeken, D. & Hoek, H. W. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr. Opin. Psychiatry 33, 521–527 (2020).
Giel, K., Schmidt, U., Fernandez-Aranda, F. & Zipfel, S. The neglect of eating disorders. Lancet 388, 461–462 (2016).
Schmidt, U. et al. Eating disorders: the big issue. Lancet Psychiatry 3, 313–315 (2016).
Bulik, C. et al. The Binge Eating Genetics Initiative (BEGIN) study. BMC Psychiatry 20, 307 (2020).
Bulik, C. M. et al. The Eating Disorders Genetics Initiative (EDGI): study protocol. BMC Psychiatry 21, 234 (2021).
Krug, I. et al. A proof-of-concept study applying machine learning methods to putative risk factors for eating disorders: results from the multi-centre European project on healthy eating. Psychol. Med. https://doi.org/10.1017/S003329172100489X (2021).
Leme, A. C. B. et al. Impact of strategies for preventing obesity and risk factors for eating disorders among adolescents: a systematic review. Nutrients 12, 3134 (2020).
Wilfley, D. E. et al. Training models for implementing evidence-based psychological treatment: a cluster-randomized trial in college counseling centers. JAMA Psychiatry 77, 139–147 (2020).
Taylor, C. B., Fitzsimmons-Craft, E. E. & Graham, A. K. Digital technology can revolutionize mental health services delivery: the COVID-19 crisis as a catalyst for change. Int. J. Eat. Disord. 53, 1155–1157 (2020).
Herman, B. K. et al. Development of the 7-item binge-eating disorder screener (BEDS-7). Prim. Care Companion CNS Disord. https://doi.org/10.4088/PCC.15m01896 (2016).
Gormally, J., Black, S., Daston, S. & Rardin, D. The assessment of binge eating severity among obese persons. Addict. Behav. 7, 47–55 (1982).
van Strien, T., Frijters, J. E. R., Bergers, G. P. A. & Defares, P. B. The Dutch Eating Behaviour Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 5, 295–315 (1986).
Fairburn, C. G. & Beglin, S. J. Eating Disorder Examination Questionnaire (6.0). in Cognitive Behaviour Therapy and Eating Disorders (ed. Fairburn, C. G.) (Guilford Press, 2008).
Garner, D. Eating Disorder Inventory-3 (EDI-3) Professional Manual (PAR, 2004).
Maguen, S. et al. Screen for disordered eating: improving the accuracy of eating disorder screening in primary care. Gen. Hosp. Psychiatry 50, 20–25 (2018).
Stunkard, A. J. & Messick, S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J. Psychosom. Res. 29, 71–83 (1985).
Yanovski, S. Z., Marcus, M. D., Wadden, T. A. & Walsh, B. T. The Questionnaire on Eating and Weight Patterns-5: an updated screening instrument for binge eating disorder. Int. J. Eat. Disord. 48, 259–261 (2015).
Fairburn, C. G., Cooper, Z., & O’Connor, M. in Cognitive Behaviour Therapy and Eating Disorders (ed. Fairburn, C. G.) (Guilford Press, 2008).
First, M. B., Williams, J. B. W., Karg, R. S. & Spitzer, R. L. Structured Clinical Interview for DSM-5–Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV) (American Psychiatric Association, 2015).
Stunkard, A. J. Eating patterns and obesity. Psychiatr. Q. 33, 284–295 (1959).
Hamburger, W. W. Emotional aspects of obesity. Med. Clin. North. Am. 35, 483–499 (1951).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders 3rd edn (American Psychiatric Association, 1980).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders 4th edn (American Psychiatric Association, 1994).
Kolar, D. R., Rodriguez, D. L., Chams, M. M. & Hoek, H. W. Epidemiology of eating disorders in Latin America: a systematic review and meta-analysis. Curr. Opin. Psychiatry 29, 363–371 (2016).
Smink, F. R., van Hoeken, D., Oldehinkel, A. J. & Hoek, H. W. Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. Int. J. Eat. Disord. 47, 610–619 (2014).
Faravelli, C. et al. Clinical epidemiology of eating disorders: results from the Sesto Fiorentino study. Psychother. Psychosom. 75, 376–383 (2006).
Bagaric, M., Touyz, S., Heriseanu, A., Conti, J. & Hay, P. Are bulimia nervosa and binge eating disorder increasing? Results of a population-based study of lifetime prevalence and lifetime prevalence by age in South Australia. Eur. Eat. Disord. Rev. 28, 260–268 (2020).
De Silva, A., Salem, V., Matthews, P. M. & Dhillo, W. S. The use of functional MRI to study appetite control in the CNS. Exp. Diabetes Res. 2012, 764017 (2012).
Heal, D. J. & Smith, S. L. Prospects for new drugs to treat binge-eating disorder: insights from psychopathology and neuropharmacology. J. Psychopharmacol. https://doi.org/10.1177/02698811211032475 (2021).
Quilty, L. C., Allen, T. A., Davis, C., Knyahnytska, Y. & Kaplan, A. S. A randomized comparison of long acting methylphenidate and cognitive behavioral therapy in the treatment of binge eating disorder. Psychiatry Res. 273, 467–474 (2019).
Acknowledgements
U.S. acknowledges salary support from the National Institute of Health Research (NIHR) Mental Health Biomedical Research Centre (BRC) at the South London and Maudsley NHS Foundation Trust and King’s College London. She is also supported by an NIHR Senior Investigator Award. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. C.M.B. is supported by NIMH (R01MH120170, R01MH124871, R01MH119084, R01MH118278, R01 MH124871); Brain and Behavior Research Foundation Distinguished Investigator Grant; Swedish Research Council (Vetenskapsrådet, award 538-2013-8864); Lundbeck Foundation (grant no. R276-2018-4581). S.Z. was supported by the publicly funded project INTERBED (01GV0601) of the German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung (BMBF)). F.F.-A. is supported by CERCA Programme/Generalitat de Catalunya for institutional support, and by research grants from PERIS (SLT006/17/00246), Instituto Salud Carlos III (PI17/01167, PI20/132, CIBERobn) and EU-H2020 grants (Eat2beNICE/H2020-SFS-2016-2, ref. 728018; and PRIME/H2020-SC1-BHC-2018-2020, ref. 847879) and COST Action (CA19115). K.S. is supported by a grant from the Margarete von Wrangell Program by the Federal Ministry of Science and Education Baden-Württemberg. K.E.G. acknowledges grants from the Federal Ministry of Education and Research (BMBF) (01KG2009) and the German Research Foundation (DFG) (GI 878/4-1). The authors thank the patient for anonymously sharing personal experiences of BED.
Author information
Authors and Affiliations
Contributions
Introduction (K.E.G.); Epidemiology (A.K.-R.); Mechanisms/pathophysiology (C.M.B. and F.F.-A.); Diagnosis, screening and prevention (K.S., K.E.G. and S.Z.); Management (P.H. and U.S.); Quality of life (P.H.); Outlook (K.E.G.); Overview of Primer (K.E.G.).
Corresponding author
Ethics declarations
Competing interests
C.M.B. received a grant from Shire, was a member of the Shire Scientific Advisory Board, acted as a consultant for Idorsia, received a grant from Lundbeckfonden, acted as an author for and received a grant from Pearson, and was a member of the Equip Health Inc. Clinical Advisory Board. F.F.-A. received consultancy honorarium from Novo Nordisk and an editorial honorarium as editor-in-chief from Wiley. P.H. is a consultant to Takeda Pharmaceuticals, receives or has received sessional fees and lecture fees from the Australian Medical Council, Therapeutic Guidelines publication, and New South Wales Institute of Psychiatry, and royalties/honoraria from Hogrefe and Huber, McGraw Hill Education, Blackwell Scientific Publications, BioMed Central and PLOS Medicine, and has received research grants from the NHMRC and ARC. She is Chair of the National Eating Disorders Collaboration Steering Committee in Australia and was a member of the ICD-11 Working Group for Eating Disorders and was Chair of the Clinical Practice Guidelines Project Working Group (Eating Disorders) of RANZCP. All views expressed in this paper are her own. All other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks M. Fennig, A. C. Grammer, C. Segura-Garcia, F. Thomas, D. Wilfey and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giel, K.E., Bulik, C.M., Fernandez-Aranda, F. et al. Binge eating disorder. Nat Rev Dis Primers 8, 16 (2022). https://doi.org/10.1038/s41572-022-00344-y
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-022-00344-y
This article is cited by
-
The cost of the perfect body: influence mechanism of internalization of media appearance ideals on eating disorder tendencies in adolescents
BMC Psychology (2024)
-
Experiences of living with binge eating disorder and facilitators of recovery processes: a qualitative study
Journal of Eating Disorders (2023)
-
SipNose-topiramate: a potential novel approach to binge eating management
Journal of Eating Disorders (2023)
-
A randomised controlled feasibility study of food-related computerised attention training versus mindfulness training and waiting-list control for adults with overweight or obesity: the FOCUS study
Journal of Eating Disorders (2023)
-
The social epidemiology of binge-eating disorder and behaviors in early adolescents
Journal of Eating Disorders (2023)



